New York
I hear it said now and again that COVID-19 is just a nasty winter bug, nothing more than a new form of flu. From what I’ve seen in New York’s intensive care units in the past few days, I can assure you this is not true. Last month I was still doing my usual job, treating patients with sleep disorders. But my training — and for many years my work — was in critical care medicine. As the coronavirus crisis developed, it was clear to me that I was needed back in the hospital, so I volunteered before the call came. Soon I was making decisions about keeping blood pressure going, when to use ventilators, whether a patient’s organ systems are functioning normally or whether support is needed. Almost every patient seemed to have remarkably rapid and severe lung injury. Most COVID-19 sufferers needed more than 70 percent oxygen — three times the level present in the air. Many struggled on 100 percent, delivered at high pressure. Dozens were on the respirator but belly down (‘proning’), a position which improves lung volumes and redistribution of the blood supply to the better-ventilated parts of the lungs. I’ve used these techniques before in Riyadh, London and Charleston, South Carolina, but not very often: lung injuries are rarely so bad. Normally, there would be — at most — two patients in an intensive care unit every few months who needed these pretty extreme techniques. In my hospital, entire units of patients are being ventilated face down, some even before we placed them on ventilators. Dozens are on extremely high levels of oxygen, even when awaiting evaluations outside the intensive care unit.
It was watching a colleague intubate a patient of mine with a ‘GlideScope’ — a fiber-optic camera that places a tube into the patient’s airway to connect them to a respirator — when I first saw the coronavirus effect. I watched on the screen. The secretions (or gunge, if you will) bubbling up from the lung were unlike that of any other disease I had ever seen. The discharge was not pink and frothy, as you see in heart failure, nor purulent, like in bacterial pneumonia. It was extremely gelatinous, thick and translucent. You could only imagine how it packs the lungs. I watched the screen longer than I should have (exposure risks are very high during an intubation procedure). The mucus looked like a monstrous creation in a Ridley Scott movie. That was when I knew this was not influenza, or anything like it.
At the end of my first week, I walked through the hallways of the Mineola New York hospital, where I had first trained in critical care medicine 24 years ago. I was disoriented and overwhelmed. Every floor now harbors multiple intensive care units. In less than a month their numbers have doubled, with more added every day. The majority of hospitalized patients have been confirmed as having COVID-19; almost a full third are critically ill. Our hospital is on target for the 50 percent increase in bed capacity that New York hospitals have been asked to achieve. Conference rooms are turned into wards, wards have become intensive care units. The number of critically ill patients in our hospital has almost trebled, with many more expected. Every ventilator we own is being used; we’ll need more. One of my colleagues knows how to set up mechanical ventilators so that they serve more than one patient (splitting has now been made lawful by Andrew Cuomo, the New York governor). It’s a relief to learn that 1,000 ventilators are being sent to New York State from China. We need all the help that we can get.
In the rare moments when I can break away from the background noise of alarms and alerts that typify every intensive care unit, I hear birdsong. This is an unusual experience in New York where there are normally competing sounds. I find myself mourning the once ubiquitous cacophony of traffic — it’s the city’s anthem.
As I walk past block after block of isolation intensive care units, I wonder: what has happened to those patients who were being treated before the pandemic? Where are the heart failure patients, the asthma exacerbations, the brittle diabetics, the deep venous thrombosis cases, the chest pains and the cases of regular pneumonia? And given what’s happened in other hospitals, I also wonder: how will my colleagues and I avoid exposure, infection, disease and even deaths among our ranks? Will we all be standing at the end? The only solace is that, between working and sleeping, there isn’t much time to indulge such thoughts.
Almost unnoticed, a New York winter entirely devoid of snow and ice has given way to a cherry-blossomed spring. This only adds to the disturbing feeling of this unfolding pandemic; the battles inside the hospitals are cast into even sharper relief by nature which marches on. I am reminded of Pablo Neruda’s poem: ‘You can cut all the flowers, but you cannot keep spring from coming.’
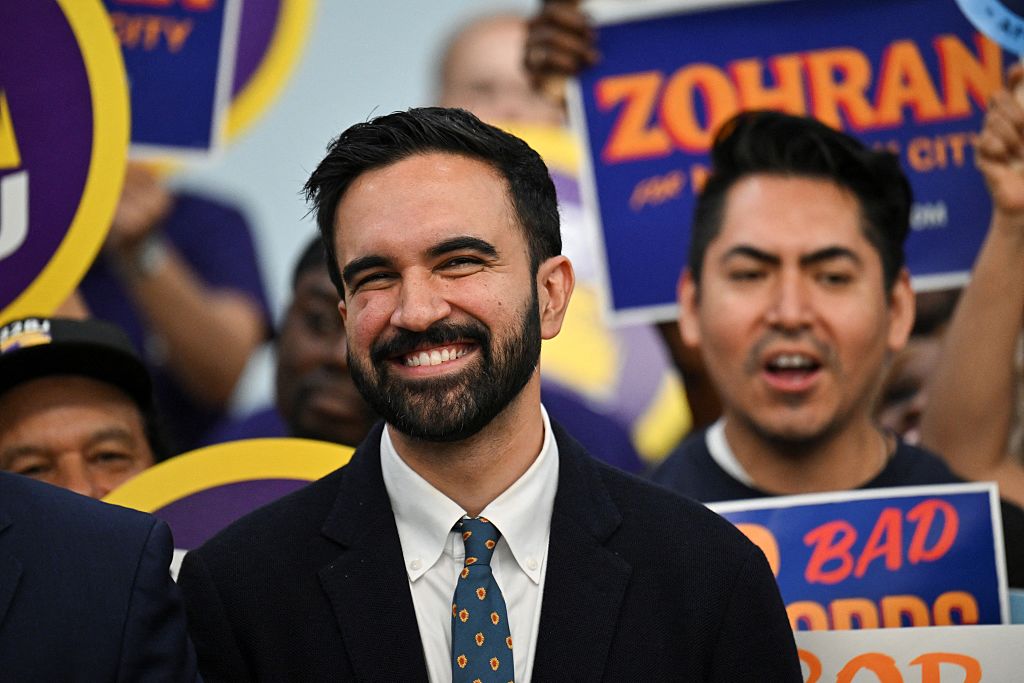
Dr Qanta Ahmed is a consultant critical care medicine physician at NYU Langone Medical Center. This article was originally published in The Spectator’s UK magazine. Subscribe to the US edition here.