I am a critical care physician and assistant professor of medicine in Canada, and have spent weeks obsessively consuming COVID-19 medical literature. Ultimately, I see only one way to navigate society through this pandemic with neither apocalyptic death rates nor economic devastation. To my surprise, the conclusion I have reached seems very similar to the ‘back to work’ plan the Trump administration floated on Tuesday.
Extreme measures to suppress COVID-19 through enforced social distancing are likely to be successful, and seem to have already succeeded in Wuhan. However, as an Imperial College London paper published last week makes clear, these measures may only work as long as they remain in place (the shaded blue area of the below chart).
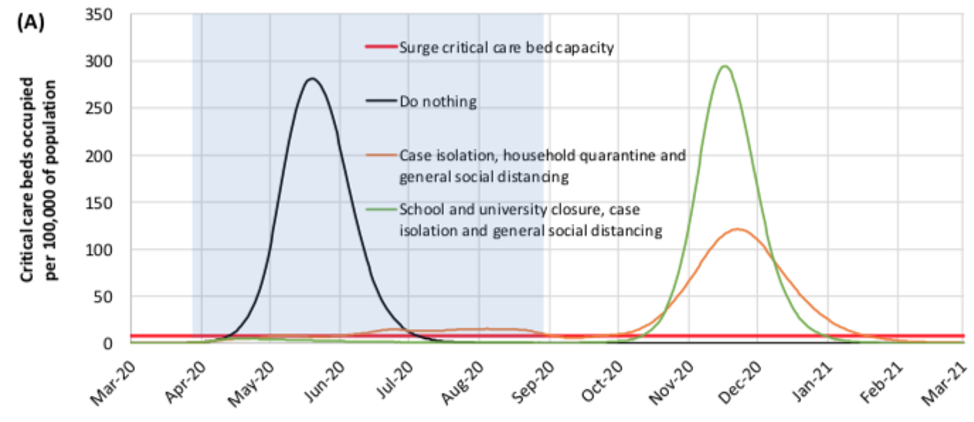
Once people begin to travel freely, engage in commerce, and send their children to school again, the epidemic could pick back up right where it left off (the green curve on the chart). Social distancing does not prevent a catastrophe, it merely buys time while we prepare and pray for a game-changer.
Some have suggested that using that delay to increase life support capacity (i.e. sourcing mechanical ventilators) in hospital intensive care units could help. Sadly, preliminary (and limited) data suggests that up to 90 percent of COVID-19 patients who go on life support will die. So ‘more ventilators’ does not seem like the game-changer we seek. As a life support specialist, myself, I am greatly chagrined to admit this.
Some, such as President Trump, hope that an old malaria drug called chloroquine will have a bigger impact. These hopes are currently based solely on anecdotal reports, and clinical trials of this and other drugs are still ongoing. But it is worth noting that 11 years after the H1N1 influenza pandemic, there are still no antiviral therapies that have been conclusively shown to save lives. This may be because of market forces, but it’s hard to believe we will succeed in finding drug therapies for COVID-19 in such a short space of time.
Lastly, there is the possibility of a vaccine being developed. The most optimistic hope is for a COVID-19 vaccine in 12 to 18 months. Let us grant, cautiously, that this is possible. Are we willing to suffer a year or more of social isolation, mass unemployment, and potential economic depression waiting for a vaccine to emerge?
I don’t think we will need to. I believe that the unique mortality profile of COVID-19 could be exploited to achieve herd immunity in a controlled and strategic manner.
At the moment COVID-19’s case fatality rate seems to be dropping. As recently as two weeks ago, The Lancet, and the WHO estimated the disease had a 2 to 3 percent mortality rate. But as widespread testing ramps up, we are finding many more cases of COVID-19 among people who do not even require hospital admission. Large countries that are performing the most COVID-19 tests per capita are seeing the lowest mortality rates.
Germany currently has identified 31,554 active COVID-19 cases, and has had 149 deaths. While in South Korea around 120 of its 9,000 COVID-19 cases have so far ended in death, leading to a crude mortality rate of 1.3 percent. This downward trajectory of the COVID-19 mortality rate has caused the prominent scientist, Dr John Ioannidis of Stanford University, to speculate that it may end up being as low as 0.05 percent.
The idea of ‘herd immunity’ has been well publicized in the past, thanks to the ongoing political controversy around the anti-vaccine movement in the United States. In the case of measles, a 95 percent vaccination rate of the population prevents outbreaks among the 5 percent who cannot be vaccinated because of their age or other medical problems. The measles virus could infect and kill those 5 percent who are unprotected, but it never gets to them because the vaccinated members of the population form a firewall that prevents the disease spreading.
The proportion of a population that has to be immune in order to confer herd immunity on the rest of the population is a function of how contagious the virus is. Data from Wuhan is still preliminary, but mercifully, COVID-19 does not appear to be as contagious as measles. Its ‘reproduction rate’ has been estimated to be as low as 2.2 (every one person who gets the disease gives it to 2.2 people), which means you would reach herd immunity when 40 to 60 per ent of the population has been infected.
If there was a way to safely grant two-thirds of a society Covid-19 immunity, the pandemic would stop.
Covid-19’s mortality profile is peculiarly age-specific. Bird flu, swine flu, SARS and MERS outbreaks were all equal-opportunity killers. They showed no mercy to the young and healthy. This does not seem to be the case with Covid-19. The crude mortality data from China by age points us in this direction:
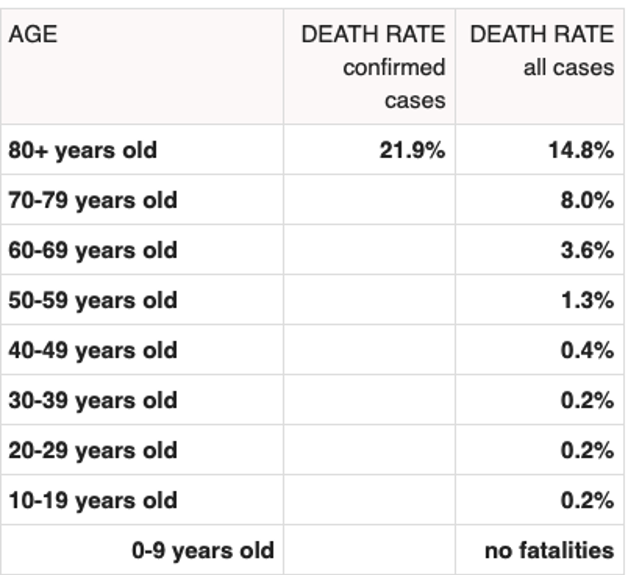
People under 50 are 25 times less likely to die of COVID-19 than people over 80. Of the 0.2 percent of young people with COVID-19 who die of the disease, it’s believed that most had some other medical problem, had minor conditions such as mild asthma, high blood pressure, were obese or smoked.
This peculiar mortality profile probably explains why Italy has had such a high case fatality rate. Italy is home to the world’s second most elderly population. These elderly citizens are famously close with their extended family, and scholars have documented high rates of intergenerational contact among them. No attempt to particularly sequester the Italian elderly was ever made.
It’s been reported that the UK planned to pursue a public health strategy of herd immunity but abandoned it after that same Imperial College report suggested it would lead to ICU bed shortages in the short term. However, the UK’s initial approach may not have taken this demographic vulnerability analysis into account. There was no real plan to completely sequester people over 50 or young asthmatics and smokers while the pandemic blew through the rest of society. The British prime minister has since ordered a nationwide lockdown of at least three weeks.
I am glad that extreme social distancing has been enforced. I do not think that either the young or the old would have taken the pandemic seriously until they saw schools and offices close. But once these measures have proven their effect, and the virus is demonstrably suppressed, public health authorities could consider ratcheting restrictions down in a way that respects demographic vulnerability. Perhaps two weeks from now, healthy people under 40 could return to work provided that they have no vulnerable people in their household. Perhaps a week after that, healthy people aged 40 to 50 could join them, and nurseries could reopen.
I have discussed this strategy here as a matter of consideration for ongoing public health conversations. I absolutely do not raise it for personal decision-making. Whether or not you are convinced of this reasoning, you do not have license to disobey public health pronouncements in your jurisdiction. But maybe, just maybe, once all the data is in and things are under control, this could be our collective way out of here.
Matt Strauss is the former medical director of the critical care unit at Guelph General Hospital, Canada. He is now an assistant professor of medicine at Queen’s University. This article was originally published on The Spectator’s UK website.